Publications IPH Magazine Revista IPH Nº17 Design Insights from a Research Initiative on Ambulatory Surgery Operating Rooms in the U.S.
- IPH Magazine #17
- COVID-19 pandemic and the trends in healthcare design: insights from the "Decalogue for Resilient Hospitals"
- Healthcare closer to people: A qualitative study of a Swedish reform on healthcare delivery
- Spatial flexibility and extensibility in hospitals designed by João Filgueiras Lima
- Design Insights from a Research Initiative on Ambulatory Surgery Operating Rooms in the U.S.
- A study on the development of the concept growth and change on hospital architecture in Japan
- A study on hospital infection control through architecture in 1980: Chapecó Regional Hospital case study
- Natural ventilation for hospitalization environments: historical aspects
- Hospital architecture and its propositions for beginners and experts
Design Insights from a Research Initiative on Ambulatory Surgery Operating Rooms in the U.S.
David Allison, Herminia Machry and Anjali Joseph - Clemson University, USA


Abstract
This paper reports on significant physical design implications and findings of a multidisciplinary iterative research-design-prototype initiative focused on the development and systematic evaluation of an ambulatory surgery operating room (OR) prototype. The overall goal of this project was to design a safer, more ergonomic, and efficient OR prototype for ambulatory surgery through evidence-based research that can inform the design of future ambulatory surgery ORs. The methodology involved initial literature and case study research, observations, and coding of surgical flow disruptions in 35 related surgical procedures, an iterative prototype design-fabrication-testing-redesign process, and ultimately a post occupancy evaluation of an operating room in a new facility that was designed in part on the results of the research. Overall findings from the study include design recommendations about OR size and layout in terms of surgical table positioning and the location of information displays and workstations.
Key words:
Surgical environment, Operating Room, Built Environment, Evidence-based Design, Prototype Development.
Introduction
Existing research, clinical practices and design guidelines for the design of surgical environments indicate that the operating room (OR) is a complex milieu with a significant potential to impact clinical outcomes for patients, safety outcomes for both patients and clinicians, and operational efficiency and effectiveness outcomes for surgical processes (ELBARDISSI et al., 2011). The numerous technical and functional forces and constraints driving OR design decisions are everchanging, often compounding and, at times, conflicting in terms of optimizing these outcomes (ROSTENBERG & BARACH, 2012). At the same time the overall physical configuration of operating rooms demonstrates little change since the mid-twentieth century, typically consisting of square or rectangular rooms with the operating table centrally located on the
axis of the room.
According to the United States Institute of Medicine, adverse events such as surgical site infections and medical errors often result from flawed systems rather than negligent clinicians (DONALDSON et al., 2000). Studies show that such adverse events occur in the OR setting as a result of everyday delays, flow disruptions, and minor errors, often overlapped and inter-related, which are in turn caused by mismatched organizational policies, processes, technology and the built environment (PARKER et al., 2010; WIEGMANN et al., 2007). Previous studies suggest that the built environment is a contributing factor to the safety and efficiency of surgical procedures due to features such as layout, lighting, acoustics and ergonomics. Certain features also potentially contribute to surface contamination and disruptions in the flow of air, people, and equipment (AHMAD et al., 2016; JOSEPH et al., 2018-I).
Environmental sources of disruption in the OR can include door openings, loud noises and alarms, environmental clutter and constrained spaces (WAHR et al., 2013; JOSEPH et al., 2018-I; JOSEPH et al., 2018-II). Coupling small and cluttered ORs with high foot traffic inside of the OR as well as movement in and out of the room may contribute to flow disruptions (e.g. people or equipment blocking visibility and communication between surgical team members) and increase infection risks (e.g. non-sterile surgical personnel bumping into a sterile instrument table) (PALMER et al., 2013; GURSES et al., 2012). Additionally, poorly organized storage spaces and the lack of proximity between key functional areas can result in unnecessary travel and time wasted during surgical procedures, ultimately causing delays and adding costs to healthcare organizations (GURSES et al., 2012; FREDENDALL et al., 2009).
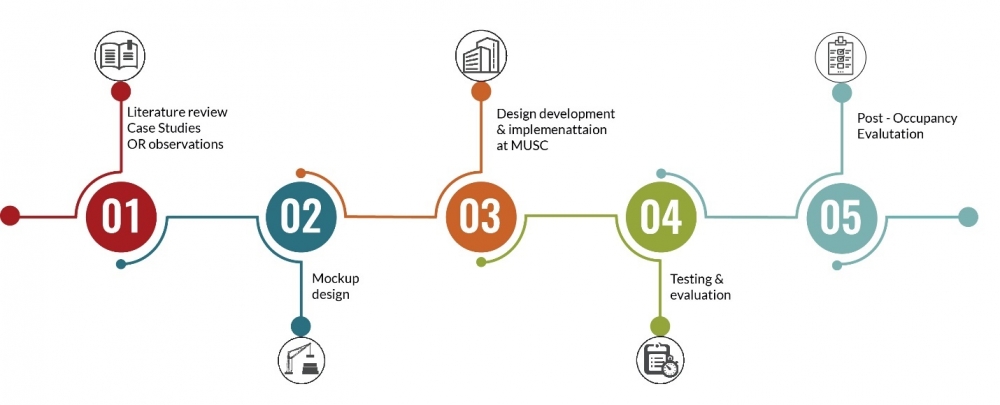
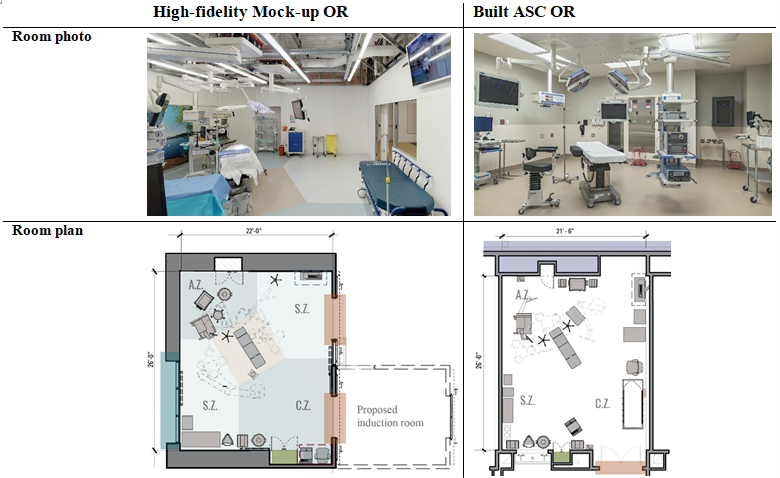
Aimed at embodying an evidence-based design process to uncover the role of the built environment in this complex OR work system, the research project presented in this paper (Realizing Improved Patient Care through Human-Centered Design in the Operating Room - RIPCHD.OR) developed a five-year multidisciplinary approach to iteratively understand, develop and evaluate OR design features impacting safety, efficiency and human experiences. Due to the multidisciplinary expertise needed to design surgical environments, the study included teams from Clemson University (Architecture, Industrial Engineering and Business departments) and the Medical University of South Carolina (MUSC). The research team included healthcare design researchers, architects, industrial designers, human factors and health professionals, healthcare providers and industry partners. As depicted in Figure 1, the research project was developed over five years, comprising an extensive multi-method problem analysis phase (year 1), the development of OR design alternatives based on the evidence found (year 2), the iterative process of evaluating and refining the design through mock-up-based simulations (year 3), and the evaluation of the final design
prototype (year 4).
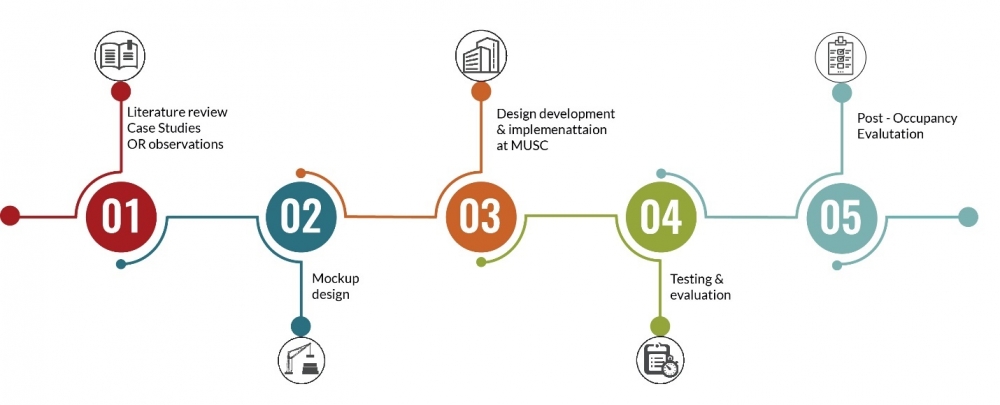
Figure 1: Timeline of the RIPCHD.OR research project
Summary of Research Methods
The RIPCHD.OR research kicked off with a review of 198 articles, which helped identify key categories of OR outcomes (e.g. disruptions, errors, satisfaction, performance) and design factors impacting those outcomes (e.g. air quality, acoustics, lighting, materials, layout, visibility). Summarized in another publication (JOSEPH et al., 2018-I), these findings helped to focus data collection efforts for the team, providing structure to the video observations and case studies being conducted. Data from the literature review, observations and case studies were used to develop several design prototype alternatives, while also informing multiple data analysis strategies such as spaghetti diagrams and discrete-event simulation models created to better understand flow patterns in the OR. The OR prototype was refined through several stages of mock-up-based simulations with end-users (surgical team members), iteratively refining the OR prototype towards its final version. The final OR prototype was then evaluated via high-fidelity simulations of surgical procedures in the physical mock-up, as well as by a computer-based simulation approach (proactive modeling) testing different versions of the prototype (different room size, shape and layout) against traffic flow patterns pre-determined in observations. Finally, ORs built in an Ambulatory Surgical Center in the Southeast US were partially informed by the research and evaluated via a Post-Occupancy Evaluation study.
Video Observations and Coding
Using a human factors systems approach (Systems Engineering Initiative for Patient Safety 2.0 - SEIPS 2.0, by HOLDEN et al., 2013), the research team observed 35 outpatient surgeries (pediatric and orthopedic procedures) conducted in five different ORs at a healthcare facility. Using video cameras installed in four corners of each OR, a coding software (Noldus Observer®) and a coding protocol developed from a previous study (PALMER et al., 2013), nine trained researchers recorded the type, location and duration of surgical flow disruptions and activities performed by key surgical team members (e.g. circulating nurse, scrub nurse, surgeons and anesthesiologists) and objects (e.g. instrument tables) in each surgery. Door openings and surgery phases were also recorded.
To optimize coding and make results more meaningful, each OR was divided into various location zones based on their functions (e.g. surgical table zone, circulating nurse workstation zone, supply zone), and activities were categorized in terms of what they related to (e.g. patient, equipment, information). Surgical flow disruptions, on the other hand, were categorized as they related to layout (inadequate use of space, impeded visibility, connector positioning or furniture positioning hindering the surgical team from doing their tasks), environmental hazards (e.g. objects causing collision/bumping or the risk of slipping/falling/tripping), usability (e.g. malfunctioning furniture and equipment), equipment failure, and interruptions (e.g. surgical team members spilling/dropping/picking up items, or searching for missing surgical items). Moreover, surgical flow disruptions were also coded in terms of their severity (from no/minor impact to momentary distraction, disruption,
and repeated task).
Case Studies and Flow Mapping
In order to more deeply investigate best practices in OR design across the United States, the research team visited three surgical facilities with varying spatial configurations and operational models, in addition to the observation site. The goal was to not only learn lessons about design and technology related facilitators and barriers to OR outcomes, but also gain insight into spaces around the OR, understanding multiple flows of people and objects feeding into the surgical procedure by traveling around the surgical suite and other areas such as the sterilization processing department. To meet these goals, the research team developed a case study tour approach that included a flow mapping tool (MACHRY et al., 2020) focused on documenting and evaluating eight different types of flows within the surgical unit (patient, family, surgeon, anesthesiologist, instruments/materials, supplies, movable equipment and waste) and how discrete steps within these flows may be impacted by spatial configuration. The tool guided interviews with stakeholders, the development of flow diagrams, and a process-based spatial evaluation framework focused on efficiency. Spaces used for traveling (e.g. elevators and corridors) or storage steps, for instance, were evaluated as to whether they were likely to present risks of delay to the next surgical case in the form of bottlenecks and/or longer distances from one step to the next.
Development and Simulations of OR Prototype and Mock-ups
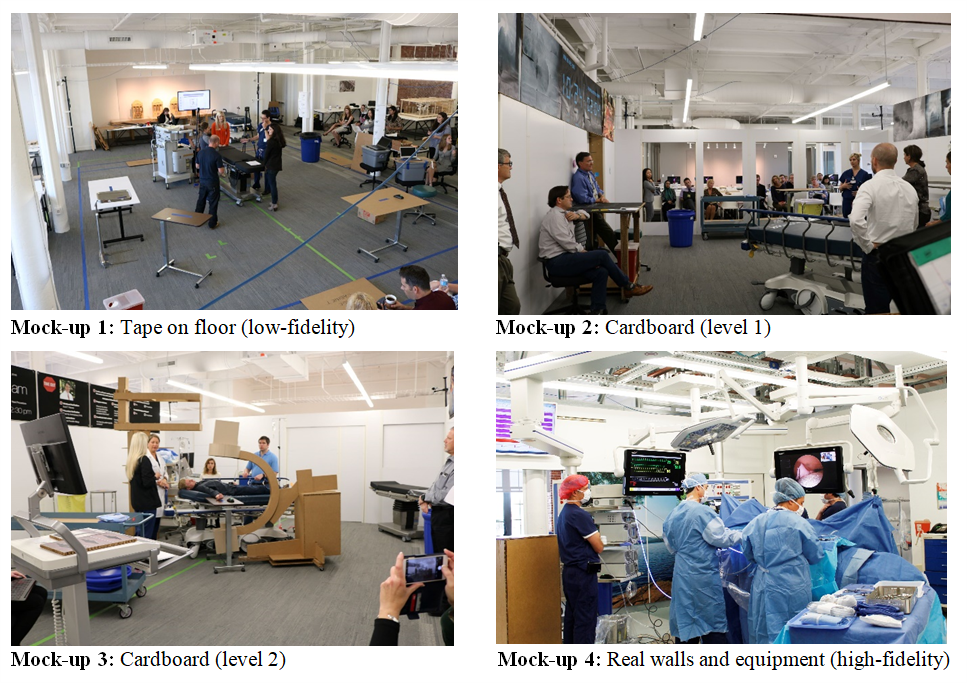
Developed in parallel to data collection, the final OR prototype and high-fidelity mock-up resulted from four intense cycles of design-fabrication-testing-redesign, in a process involving the cross disciplinary research team, an advisory committee and graduate students. The initial task was to collectively build an evidence-based framework to guide the design of the prototype (Figure 3 in the next section). This was done based on the literature review and workshops bringing the entire team together to filter evidence and best practices relevant to the project. After reaching consensus and clarity on the design vision and guidelines to focus on, several design solutions were developed, narrowed down, and replicated in a low-fidelity tape on the floor mock-up.
Flexible enough to reflect various design alternatives, the first tape-on-the-floor mock-up was tested through a set of simulations with end-users used to refine the design. This mockup confirmed basic room floor area and dimensions. It also tested several potential door locations. As depicted in Figure 2, this process was repeated two more times with cardboard mock-ups, allowing for a dramatic reduction in the number of design alternatives being tested each time, and ultimately leading to the development of the final version of the prototype to be reproduced in a high-fidelity mock-up with real walls and surgical equipment.
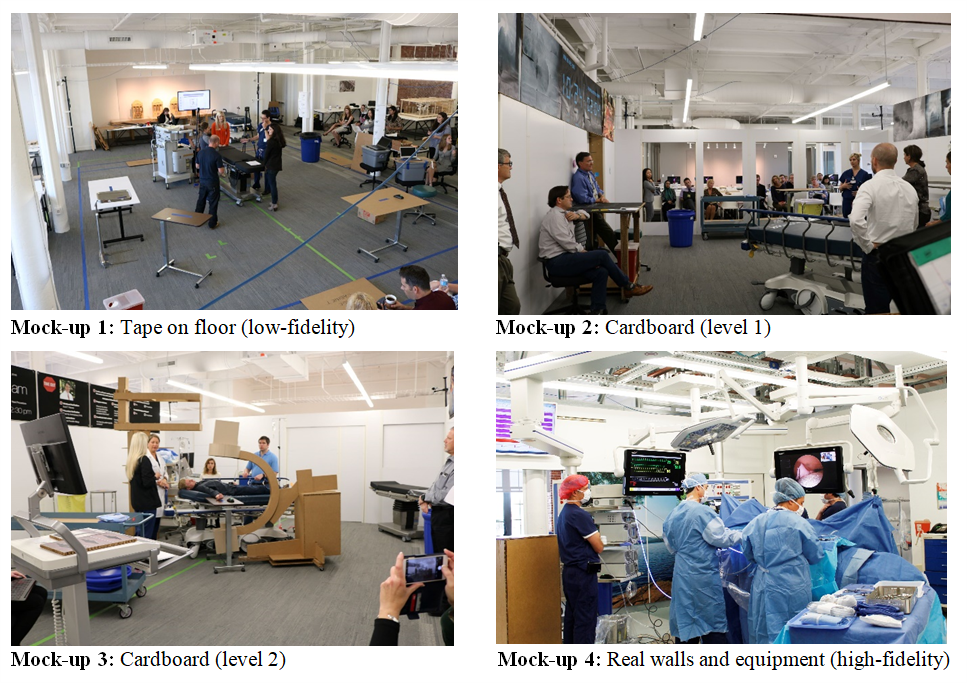
Mock-up 1: Tape on floor (low-fidelity); Mock-up 2: Cardboard (level 1); Mock-up 3: Cardboard (level 2) Mock-up 4: Real walls and equipment (high-fidelity)
Figure 2: Four stages of mock-up development.
Structured around the prototype design and mock-up fabrication, simulations were developed to test OR design alternatives in each stage described above, with simulation results informing the redesign of the prototype in the next stage. A set of tools was adapted from the Health Quality Council of Alberta (HQCA, 2016) to evaluate each simulation, testing the design against guidelines established in the project's framework (test whether the design was able to optimize movement and flow, for example). Based on the HQCA structure and assisted by clinicians in the research team, a simulation-based evaluation toolkit was developed with simulation scenarios and protocols that were tailored to simulate surgical tasks and sequences (BAYRAMZADEH et al., 2017). Scenarios depicted different types of ambulatory surgery procedures (specific pediatric and orthopedic surgeries), surgery phases (preoperative, perioperative, postoperative and turnaround phases), and OR configurations (e.g. with one or two doors; with or without adjacent rooms such as the induction room). Always including end-users (e.g. surgeons and nurses), each simulation protocol defined a simulation director, participant roles and tasks, equipment and tools involved, and a simulation schedule involving a sequence of discrete/shorter simulations (e.g. patient bed entry/exit sequences). Each simulation was followed by debriefings and focus groups to discuss perceptions and lessons learned from the simulation right after it happened.
As the quality and fidelity of mock-ups improved, so did the level of detail in simulation scenarios (e.g. tasks including specific furniture/equipment becoming available in higher-fidelity mock-ups) and evaluation tools. During the first two rounds of simulations (mock-ups 1 and 2), conclusions were essentially drawn based on content analysis of debriefing notes, observation notes and annotated sketches and floor plans. The third round of simulations (mock-up 3) deployed more structured and detailed scenarios, tasks, observations and evaluation questions (see details in another publication - BAYRAMZADEH et al., 2017). The final round of simulations, on the other hand, was more detailed due to the high level of fidelity of the mock-up (mock-up 4), and included longer uninterrupted simulations (entire surgery as opposed to discrete parts of it) and video observations. Thus, more advanced data collection procedures were utilized in the final round of simulations, including surveys, behavior mapping and coding (e.g. tracking movement and surgical flow disruptions), and focus groups.
Computer-based Simulations of the OR Prototype
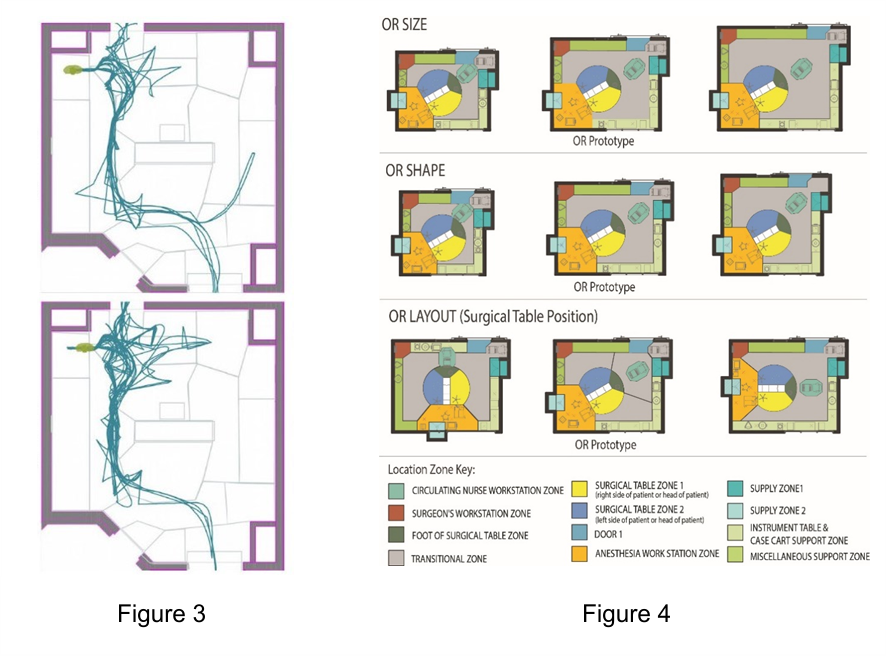
Once the final design of the OR prototype was defined and built in the high-fidelity mock-up, a digital simulation method was deployed to manipulate some of its features (size, shape and layout) and test their performance against the flow patterns obtained from coding video observations of actual surgeries (Figure 3). As explained in detail in another publication (TAAFFE et al., 2020), a computer-based simulation modeling approach was created to simulate these flow patterns in the different versions of the OR prototype (Figure 4). Different OR sizes (421, 579 and 739 square feet or approximately 39, 54 and 68 square meters), shapes (square and rectangle) and layout (surgical table positioned perpendicularly or angled to OR walls) were compared to see how they performed in terms of flow measures impacting safety and efficiency during surgery - the number of contacts between people/equipment, the distance traveled by surgical team members, and the number of transitions near the surgical table area.
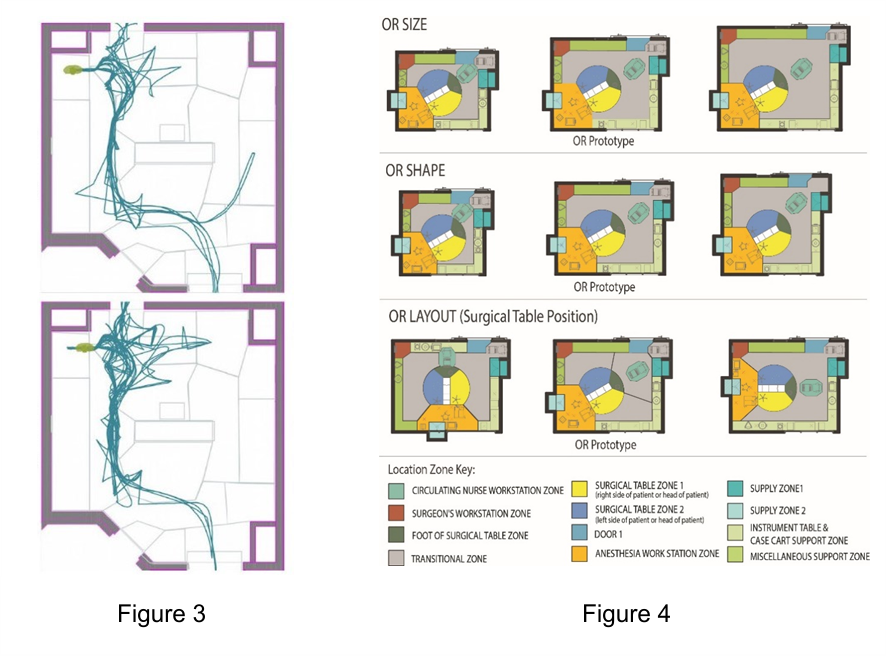
Figure 3: Spaghetti diagrams depicting flow patterns obtained from coding video observations of 35 surgeries.
Figure 4: Manipulations of the OR prototype in terms of size, shape and layout that were tested against proactive simulations of flow patterns.
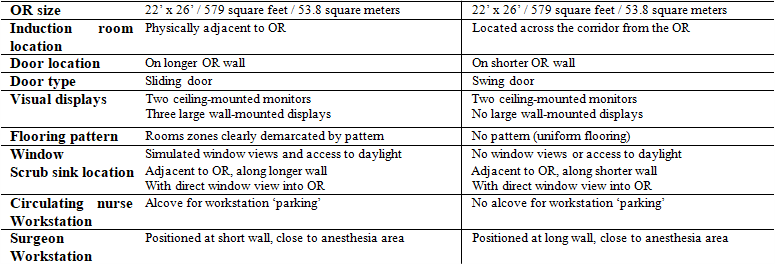
Post-Occupancy Evaluation of Built Facility
Completing the evidence-based cycle of the research, a post-occupancy evaluation (POE) was conducted to further evaluate design features of the OR prototype during actual surgical procedures. Largely designed to reflect findings from the aforementioned simulations, the ORs built in the Ambulatory Surgery Center (ASC) were similar to the OR prototype in overall size and layout (e.g. location/position of the surgical table), and different in terms of features such as the number and position of doors and information displays. See Figure 5 comparing both rooms.
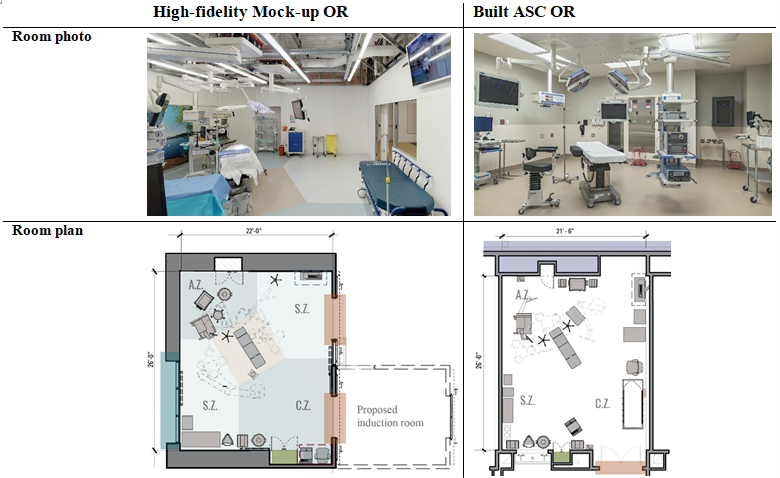
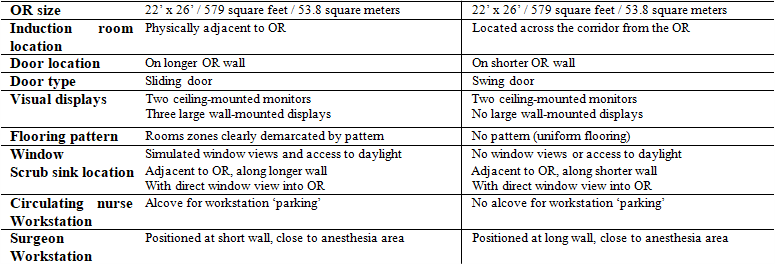
Figure 5: Comparison between OR prototype and built ASC OR.
Replicating some data collection procedures previously described (video observations, coding, flow mapping, surveys and focus groups), POE results were compared to simulation results from the high-fidelity mock-up.
Architecturally Relevant Findings
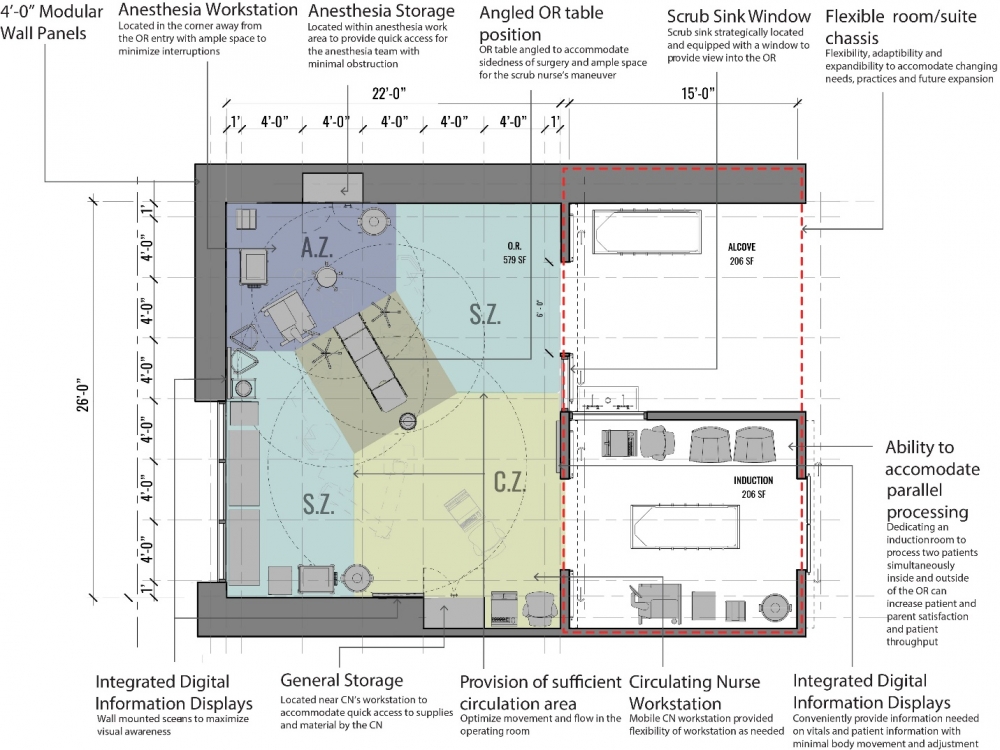
A major outcome from the initial phases of this research (literature review, video observations and brainstorming workshops) is the confirmation of a project vision and a series of evidence-based design goals and guidelines. A set of five evidence-based goals -1) optimize operational efficiency and effectiveness, 2) optimize clinical outcomes, health and safety, 3) optimize the experience for both patients and staff, 4) optimize green and sustainable practices, and 5) optimize the ability to accommodate changing needs over time - led to a series of nine inter-related OR design guidelines - optimize movement and processes, maximize visual awareness, integrated information display, minimize institutional clutter, minimize surface and airborne contamination, controlled access to daylight and appropriate artificial lighting for the range of activities in the OR, and a flexible room/suite chassis with flexible and interchangeable plug and play elements. See Figure 6 illustrating the framework guiding the design of the OR prototype, which is then depicted as a floor plan on Figure 7.

Figure 6: Diagram of framework guiding the design of the OR prototype.
OR Size and Shape
The overall net dimension of the final OR prototype was 22' x 26' or approximately 6.7 x 7.9 meters. With an alcove for parking a circulating nurse workstation and storage, the net area of the room ended up being 579 square feet or 53.8 square meters. As described earlier, this area and dimension were evaluated in simulation models compared to larger and smaller room areas and dimensions. Findings from simulations (both mock-up-based and computer-based) indicate the prototype room size and dimensions performed well in terms of flow patterns and disruptions, showing fewer incursions into the sterile zone than smaller rooms and fewer travel/steps than larger rooms (TAAFFE et al., 2020).
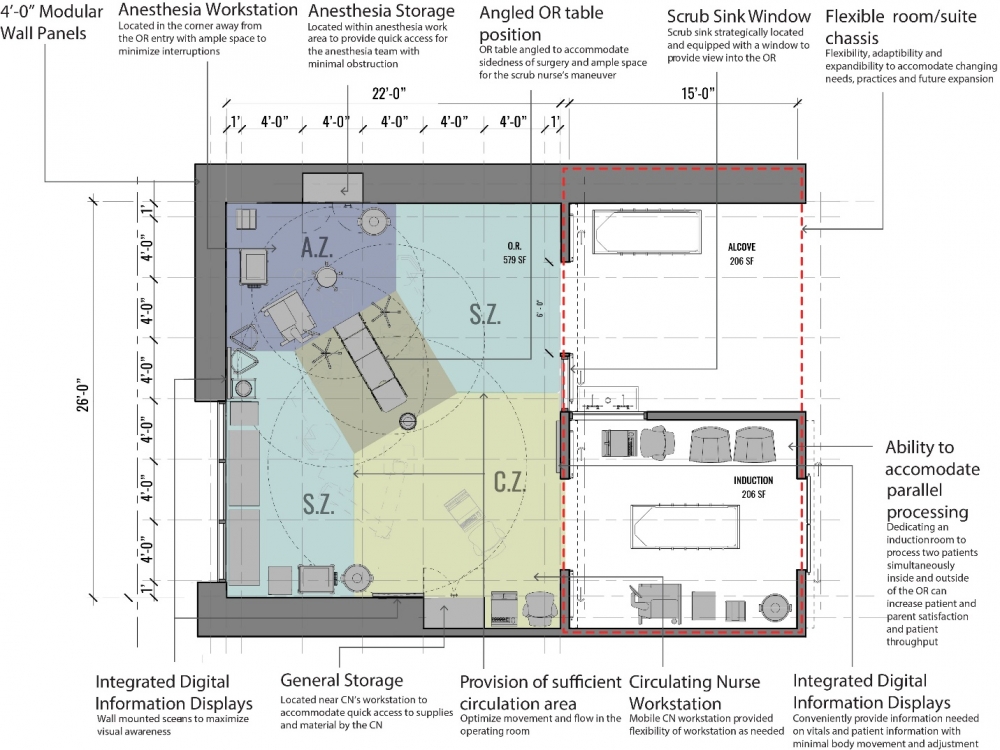
Figure 7: Annotated floor plan of the final OR prototype.
OR Layout
The OR prototype is fundamentally organized into four designated zones around the sterile field at the OR table: an anesthesia work zone (AZ) at the head of the table, surgical work zones (SZ) on either side depending on left or right-side surgeries and a circulating zone (CZ) at the foot and entry corner of the room. These zones were demarcated in the prototype by flooring colors, which facilitated the surgical flow according to focus groups. The surgical table placement and orientation off center and diagonal in the room opens up the foot and side areas around the table for circulation, equipment and procedure setup while placing the anesthesia work area so that it is more protected and less prone to movement through it by other surgical team members. According to simulations and the POE, such atypical positioning of the surgical table also allows for more efficient and effective use of space in the room by eliminating the need to access space typically found in the far corner of the room, behind the anesthesia boom and between the primary surgical zone and anesthesia zones, which otherwise would be accessed by passing through either the anesthesia or surgeon workstation zones. Furthermore, research findings showed that the surgical table orientation and placement away from the patient entry door facilitates maneuvering and minimizes effort during patient bed flow in and out of the room.
Mobile Circulating Nurse Workstation
Based on feedback from mock-up-based simulations, the OR prototype proposed a mobile circulating nurse workstation that allows flexibility for the position of the nurse during surgery, therefore facilitating repositioning based on visibility and flow needs, irrespective of the surgical table orientation. This enables the circulating nurse to optimally position the workstation to view the procedure while documenting or monitoring the surgery in the computer. A parking alcove is provided for this workstation when it is not in use (e.g. during turnaround or postoperative phases). Observations and focus groups also highlighted the importance of cord management, outlet positioning, and the location of environmental control devices (e.g. lighting) when it comes to the mobile workstation, since it requires a power outlet for charging and some staff reported preference for having the workstation plugged in at all times.
Information Displays
The OR prototype was designed with integrated patient information retrieval and display technology in addition to adjustable boom mounted displays around the surgical table. Proposed wall-mounted information displays were located on three walls of the prototype, envisioning a continuous band of digital display integrated into the wall panels surrounding the entire room. The prototype was fabricated with three wall mounted monitors: one on each long wall and one on the footwall of the room. Aiming to enhance situational awareness, displays were positioned to allow optimal visibility for the entire surgical team at any time during the surgery, on either side of the surgical table, and while moving around the room. Simulations found that displays were initially installed too high for comfortable viewing and sight lines were blocked from some points by overhead surgical booms and lights.
OR Flexibility
The basic room chassis of the OR prototype was designed to accommodate various suite configurations, including a clean core for storage of sterile supplies requiring access from the side of the OR opposite the general patient-staff corridor. Based on observations at one of the case studies visited, the prototype chassis was designed to accommodate the option of an adjoining induction room for pediatric cases. Given most pediatric surgeries are of a short duration with a longer preoperative stage involving induction, this allows the next case to begin the induction process with a separate anesthesia team outside of the OR while a procedure was still in progress. This enables parallel processing with quicker turnaround times and throughput of surgical cases in a given day. The separate induction room also allows family members to be with the child during the intimidating induction process without the need for gowning.
Simulations showed that the configuration of the OR prototype was able to accommodate these different configurations with minor changes, incorporating adjoining ancillary rooms such as an induction room or postoperative instrument breakdown room, and a scrub sink/entry alcove. The prototype was tested in simulation for both postoperative instrument breakdown associated with orthopedic surgeries and induction outside the OR for pediatric surgery. The induction room scenarios were viewed as beneficial for short duration pediatric cases and ultimately adopted in the subsequently built facility as a means to improve room turnover and overall productivity.
The prototype was built with a modular and adaptable overhead structural frame to support surgical booms, surgical lights and other ceiling-mounted items (Figure 8). It was designed to enable the relocation of these overhead elements with minimal effort and cost. The simulations did not explicitly evaluate the original placement of overhead surgical booms and lights although anecdotal feedback indicated there were some difficulty in optimally positioning the surgical boom and lights across different procedures and clinician positioning. Insights indicated that the mounting locations of the booms were too close to the center of the OR table and would be better placed further apart to minimize conflicts in boom rotations.

Figure 8: Overhead boom and light structure
Applied but Untested OR features
Like the modular ceiling structure, a simulated window was included in the prototype but not tested in the research study, considering it did not face an outdoor area and was not able to simulate the experience or exposure to daylight. Nonetheless, the window was included in the prototype based on anecdotal evidence that shows how windows with appropriately controlled daylight, privacy and thermal controls were both desirable and beneficial for surgical team members. It is also speculated that windows with daylight and views could be stress reducing for ambulatory surgery patients, which is especially relevant with the increase in minimally invasive surgeries and the progress in anesthesia strategies. This suggests that more patients in the future may maintain some level of consciousness for at least periods of time in the OR, potentially increasing the need for positive distractions in the room.
The OR prototype also included sliding doors which are common in some countries but have not had widespread adoption in the US. It is speculated that sliding doors reduce effort, flow disruptions and air turbulence in the OR, but these features were also not evaluated in simulation. Likewise, overall room lighting concepts were conceived in the design but not incorporated or evaluated in simulations. The prototype was designed to minimize institutional clutter, unnecessary articulations in surfaces and minimize unnecessary horizontal surfaces to ease cleanability and potentially reduce surface contamination. Again, these features were not tested.
Conclusions
The size, dimensions and configuration of the OR prototype enabled an effective and efficient use of its space. As a major finding validated by simulations as well as the POE, placing the surgical table diagonally and off-center in the rectangular shaped room, away from the entry door, improved movement and flow in the OR, facilitating patient entry, transfer and positioning. Additionally, this position of the surgical table facilitates movement around the room without interference with the anesthesia and sterile zones around the patient, therefore avoiding flow disruptions in these areas, such as bumps, trips, and related safety risks for patients and staff. The prototype design was also successful in improving situational awareness with the location and orientation of the surgical table, the mobile nurse workstation, and multiple wall-mounted information displays. Combined, these features enabled ample visibility between surgical team members and facilitated movement for the circulating nurse, a critical role supporting the entire surgical procedure. As charging capacity and reliability improves, control devices become more available on wireless devices and smart system integration becomes more widely adopted, therefore increasing the flexibility and capacity to position and operate mobile workstations in the OR.
Simulations of the prototype mock-up indicated that the overall room design provides flexibility for a variety of pediatric and orthopedic ambulatory procedures requiring different surgical teams, equipment and positioning of the procedure and team members. Other features of the prototype that were not tested are anticipated to enable room chassis standardization with component flexibility and adaptability over the life of the room. Significant features for flexibility include a structural mounting system in the ceiling that can enable the easy repositioning of structural support and placement of overhead surgical booms and lights. Modular plug and play stainless steel wall panels are designed to allow for reconfiguration of wall integrated and mounted systems and enable repair quickly and cleanly with minimal downtime and disruption.
Limitations
Most of the limitations on evaluating the prototype design were known at the outset and framed by the scope of the study, schedule, budget and mock-up site. The prototype evaluations were focused on a limited set number of ambulatory pediatric and orthopedic surgical procedures. Several architectural design features of the OR prototype were not evaluated due to a variety of limitations. The research did not study issues of overall room lighting or evaluate the configuration of overhead booms and surgical lights. Due to the nature of simulations and overall constraints of space, time and funding, the prototype did not include mechanical systems, nor could actual surgical procedures be performed for obvious reasons, so therefore the study did not evaluate the mockup design in terms of infection control. Based on similar limitations, the study did not evaluate the impact of artificial lighting scenes, daylight or connections to nature for either patients or staff, even though considerable attention went into considering these attributes in the prototype design. Likewise, the study could not test issues of flexibility beyond accommodating the select range of pediatric ambulatory surgery procedures. These issues all deserve further consideration and evaluation in the future.
Bibliography
AHMAD, N., HUSSEIN, A. A., CAVUOTO, L., SHARIF, M., ALLERS, J. C., HINATA, N., ... & GURU, K. A. Ambulatory movements, team dynamics and interactions during robot-assisted surgery. BJU international, 2016, 118(1), 132-139.
BAYRAMZADEH, S., JOSEPH, A., ALLISON, D., SHULTZ, J., & ABERNATHY, J. Using an integrative mock-up simulation approach for evidence-based evaluation of operating room design prototypes. Applied Ergonomics, 2018, 70, 288-299. doi:https://doi.org/10.1016/j.apergo.2018.03.011
ELBARDISSI, A. W., & SUNDT, T. M. Human factors and operating room safety. The Surgical clinics of North America, 2011, 92(1), 21-35.
FREDENDALL, L. D., CRAIG, J. B., FOWLER, P. J., & DAMALI, U. Barriers to swift, even flow in the internal supply chain of perioperative surgical services department: A case study. Decision Sciences, 2009, 40(2), 327-349.
GURSES, A. P., KIM, G., MARTINEZ, E. A., MARSTELLER, J., BAUER, L., LUBOMSKI, L. H., ... & THOMPSON, D. Identifying and categorizing patient safety hazards in cardiovascular operating rooms using an interdisciplinary approach: a multisite study. BMJ Qual Saf, 2012, 21(10), 810-818.
HOLDEN, R. J., CARAYON, P., GURSES, A. P., HOONAKKER, P., HUNDT, A. S., OZOK, A. A., & Rivera-Rodriguez, A. J. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics, 2013, 56(11), 1669-1686.
HQCA. Simulation-based Mock-up Evaluation Framework. Calgary, Alberta, Canada: Health Quality Council of Alberta (HQCA), 2016. Available from www.hqca.ca/humanfactors.
DONALDSON, M. S., CORRIGAN, J. M., & KOHN, L. T. (Eds.). To err is human: building a safer health system (Vol. 6). National Academies Press, 2000.
JOSEPH, A., BAYRAMZADEH, S., ZAMANI, Z., & ROSTENBERG, B. Safety, performance, and satisfaction outcomes in the operating room: A literature review. HERD: Health Environments Research & Design Journal, 2018 (I), 11(2), 137-150.
JOSEPH, A., KHOSHKENAR, A., TAAFFE, K. M., CATCHPOLE, K., MACHRY, H., & BAYRAMZADEH, S. Minor flow disruptions, traffic-related factors and their effect on major flow disruptions in the operating room. BMJ quality & safety, 2018 (II). doi:10.1136/bmjqs-2018-007957
MACHRY, H., JOSEPH, A., & WINGLER, D. The Fit Between Spatial Configuration and Idealized Flows: Mapping Flows in Surgical Facilities as Part of Case Study Visits. HERD: Health Environments Research & Design Journal, 2020, 1937586720928350.
PALMER, G., ABERNATHY, J. H., SWINTON, G., ALLISON, D., GREENSTEIN, J., SHAPPELL, S., ... & REEVES, S. T. Realizing improved patient care through human-centered operating room design a human factors methodology for observing flow disruptions in the cardiothoracic operating room. The Journal of the American Society of Anesthesiologists, 2013, 119(5), 1066-1077.
PARKER, S. E. H., LAVIANA, A. A., WADHERA, R. K., WIEGMANN, D. A., & SUNDT, T. M. Development and evaluation of an observational tool for assessing surgical flow disruptions and their impact on surgical performance. World journal of surgery, 2010, 34(2), 353-361.
ROSTENBERG, B., & BARACH, P. R. Design of cardiovascular operating rooms for tomorrow's technology and clinical practice-Part 2. Progress in Pediatric Cardiology, 2012, 33(1), 57-65.
TAAFFE, K., JOSEPH, A., KHOSHKENAR, A., Machry, H., Allison, D., & Reeves, S. T. Proactive Evaluation of an Operating Room Prototype: A Simulation-Based Modeling Approach. Journal of Patient Safety, 2020.
WAHR, J. A., PRAGER, R. L., ABERNATHY III, J. H., Martinez, E. A., Salas, E., Seifert, P. C., ... & Sanchez, J. A. (2013). Patient safety in the cardiac operating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation, 2013, 128(10), 1139-1169.
WIEGMANN, D. A., ELBARDISSI, A. W., DEARANI, J. A., DALY, R. C., & SUNDT III, T. M. Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery, 2007, 142(5), 658-665.
Send by e-mail:


