Publications IPH Magazine IPH Magazine #16 Health financing systems worldwide

- An analysis of the sectorization and comfort in contemporary children's hospitals
- "Casinha": The story of the Birth Center in Rio de Janeiro that became a model for humanized labor and resistance to the hardships of public management
- Risk of infections caused by the presence of the fungus Aspergillus.sp: remodeling hospitals and climatization systems
- Health financing systems worldwide
- A pathway for death: the flow and connections between environments and its occupants
Health financing systems worldwide
Claudia Kodja
Besides the current difficulties, health financing systems around the world will have to deal with new challenges concerning the rise in life expectancy, the increase of non-communicable diseases and the use of new technologies.
Life expectancy
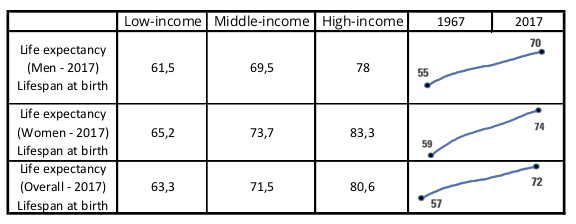
The average life expectancy has increased worldwide, from 57 years old, in 1967, to 72 years old, in 2017. A 26% variation or an increase of 15 years in lifespan.
An analysis of the increase in life expectancy
Variation between gender and income
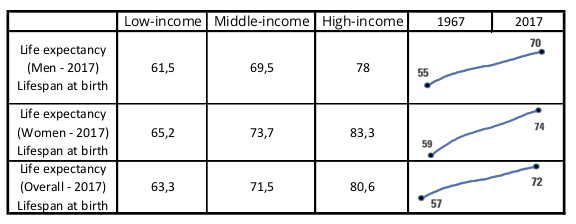
Credit: Claudia Kodja - Database: World Bank - https://data.worldbank.org/indicator
The most significant increase was seen in the low-income group, where life expectancy skyrocketed from 42,6 to 63,3 years old in that period. The group comprises about 733 million people, who still rely only on a negligible amount of the financing resources aimed at healthcare.
Non-communicable Diseases
The number of non-communicable diseases (NCD) have significantly increased over the last past years, and the reasons for that could either be the rise in life expectancy or change of habits.
In 1990, NCDs were responsible for 43% of all deaths and, in 2017, they killed 41 million people, representing 71% of all deaths around the world. Cardiovascular diseases were responsible for most deaths, killing 17,9 million people per year, followed by cancer (9 million), respiratory diseases (3,9 million) and diabetes (1,6 million).
A recent analysis carried out by the World Economic Forum shows that Brazil, China, India and Russia annually lose more than 20 million people from their workforce to NCDs.
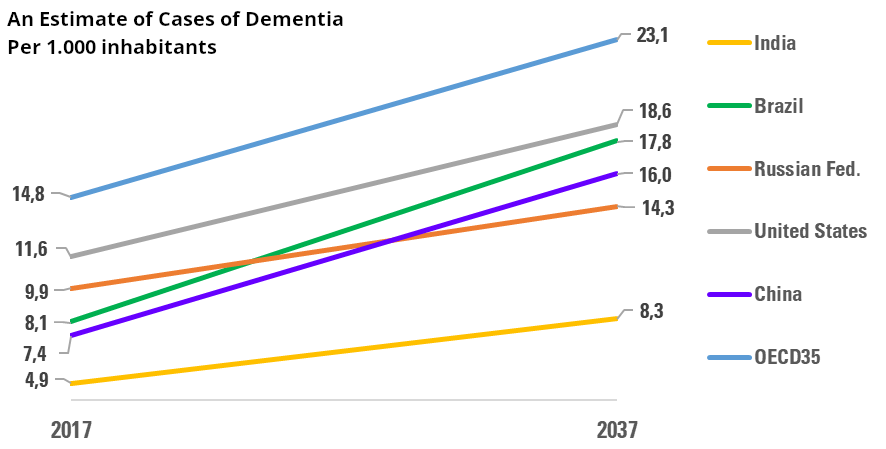
Another relevant variation, which impacts the structure of cost and services, concerns an estimate growth in dementia cases.
There are about 50 million people worldwide suffering from dementia, and almost 60% of them live in low or middle-income countries. Every year there are about 10 million new cases.
The total number of people with dementia may get to 82 million in 2030 and 152 million in 2050 (World Health Organization).
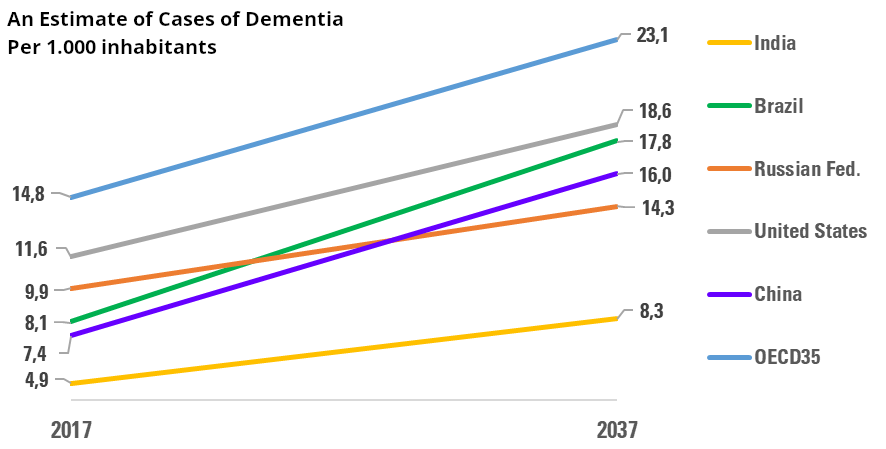
Credit: Claudia Kodja - Database: OECD. Stat - Better Life Index - https://stats.oecd.org/
Technology
Amid our current technological revolution, biotechnology and healthcare are drawing great part of the entrepreneurial venture capital to support and accelerate companies, aiming at fast growth.
Artificial intelligence, process automation and virtual reality are the medical fields that most draw entrepreneurial capital. Artificial intelligence developments for the medical area has led to the establishment of an astonishing number of startups.
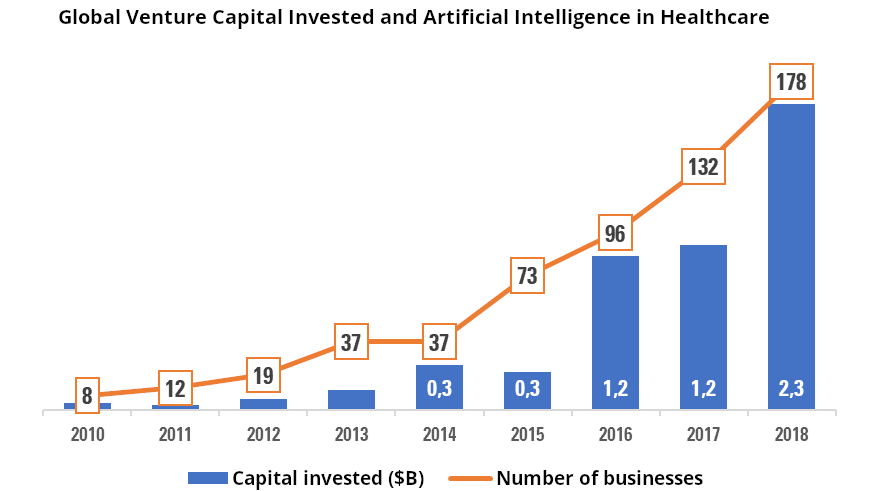
Source: KPMG Venture Pulse 2018 - KPMG Enterprise - access: May/2019 - kpmg.com/venturepulse
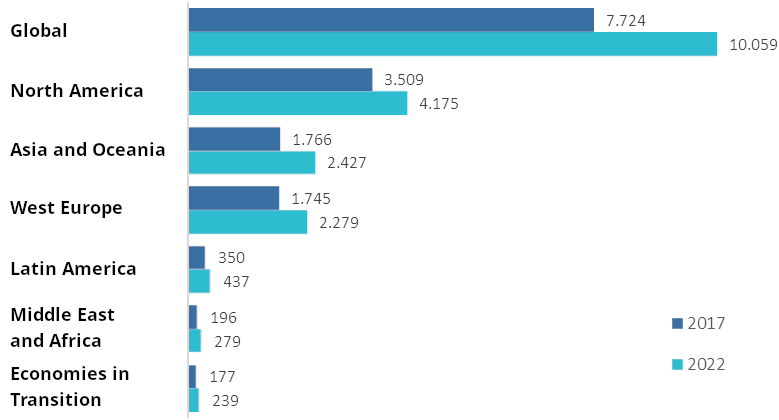
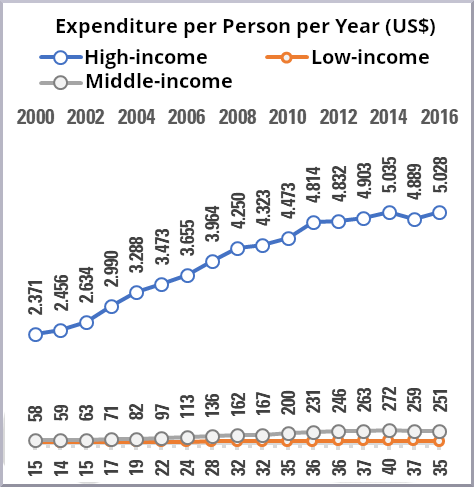
Health expenditure is growing faster than the GDP worldwide. In low and middle-income countries, annual costs have reached 6%, in high-income nations, 4%. The reasons for that can be both the structural changes necessary to comply with the increase of life expectancy, non-communicable diseases and new technologies; and the way the area itself is operating.
Spending on health may reach US$ 10.059 trillion until 2022.
Increase in Health Expenditure - 2017 to 2022 - US$ trillion
A variation of 30,2% in 5 years, roughly US$ 2.335 trillion
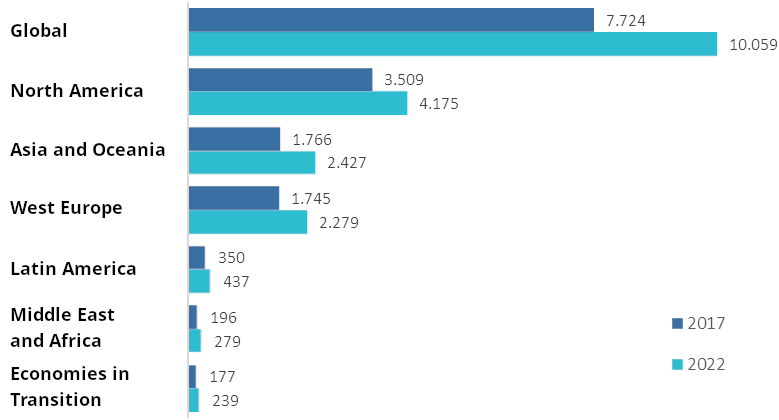
Source: 2019 Global Healthcare outlook - Deloitte Center of Healthcare Solutions
Inequality and Inefficiency in Allocating Health Resources
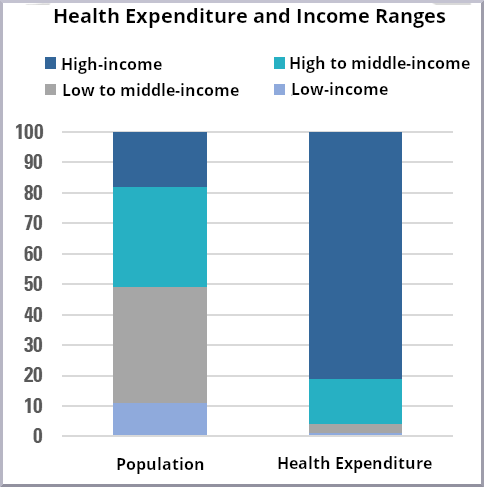
Although 80% of the world population live in low or middle-income countries, this group represents less than 20% of the total spending on health.
Such inequality is not showing signs of change and there is no guarantee new technologies will reduce the costs or ever become accessible to the low-income population.
The next pair of tables is quite elucidative to dimension what it means inequality in the contemporary economy.
 |
 |
Credit: Claudia Kodja - Database: World Bank https://data.worldbank.org/indicator.
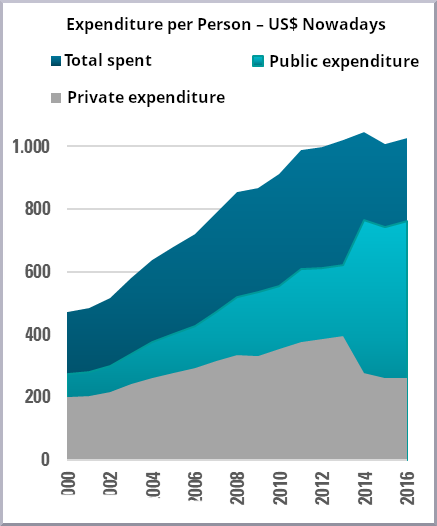
Such analysis of the amount of public and private resources invested in healthcare reinforces not just the inequality, but also the fiscal inefficiency and lack of prioritization of public health among the most vulnerable groups.
Globally, public spending on healthcare has seen a real growth of 2% thanks to the increase in investments from high-income countries. In low-income countries, public health spending has withdrawn 11% between 2006 and 2016.
 |
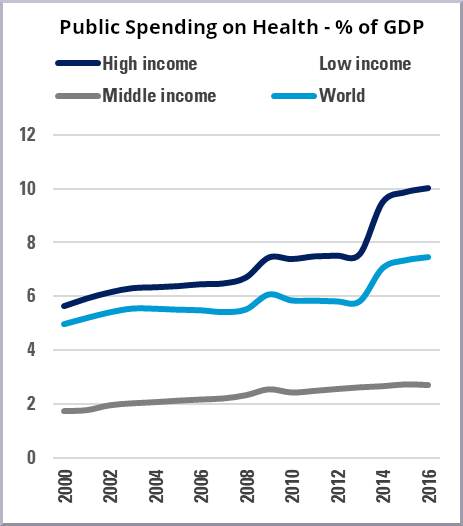 |
Credit: Claudia Kodja - Database: World Bank - https://data.worldbank.org/indicator.
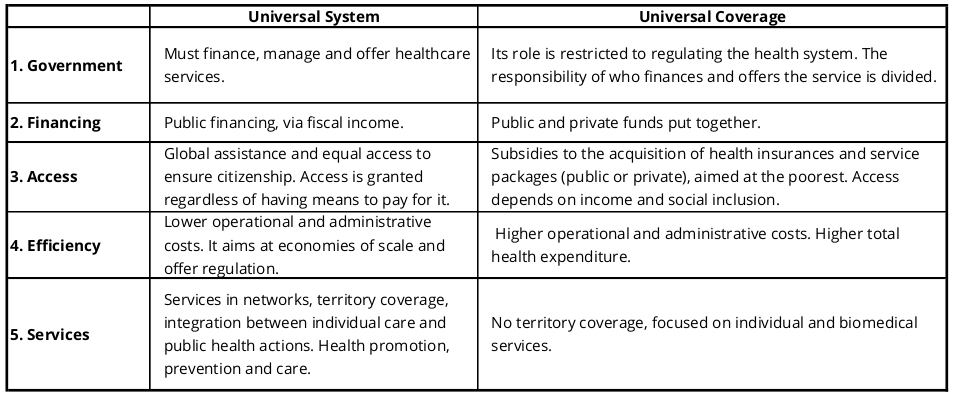
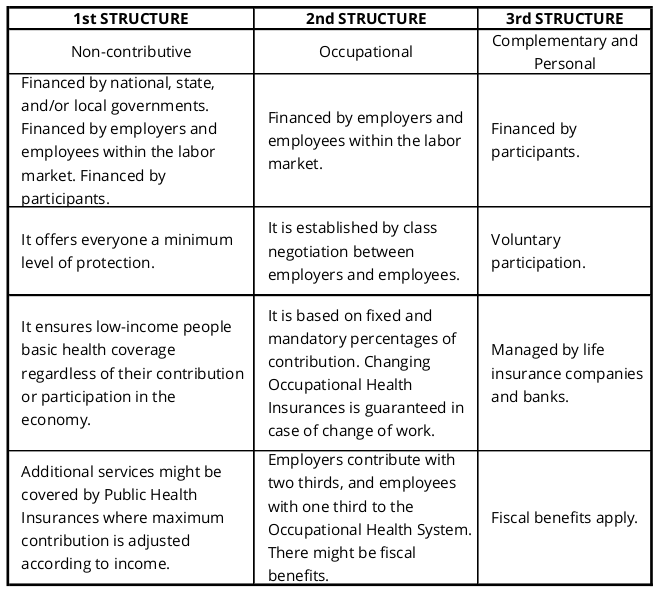
Between the Universal Health System and the Universal Health Coverage - Or Neither
The international debate concerning health financing structures bring face to face the universal system and the universal coverage. Both alternatives differ on the level of government responsibility in developing and providing healthcare.
The Universal System reflects a welfarism attitude while considering health a right every citizen must be entitle to and ensures free and global access for the society as a whole.
Universal Coverage adopts a liberal viewpoint, limiting the government role as a regulator of the health system, one that must delegate to the market the investment, maintenance and distribution of healthcare services.
Such difference could be classified as political if the access to and quality of healthcare services were not related to practical issues, such as, territory coverage, social equity and availability of resources.
Universal Health System & Universal Health Coverage
Characteristics and Differences
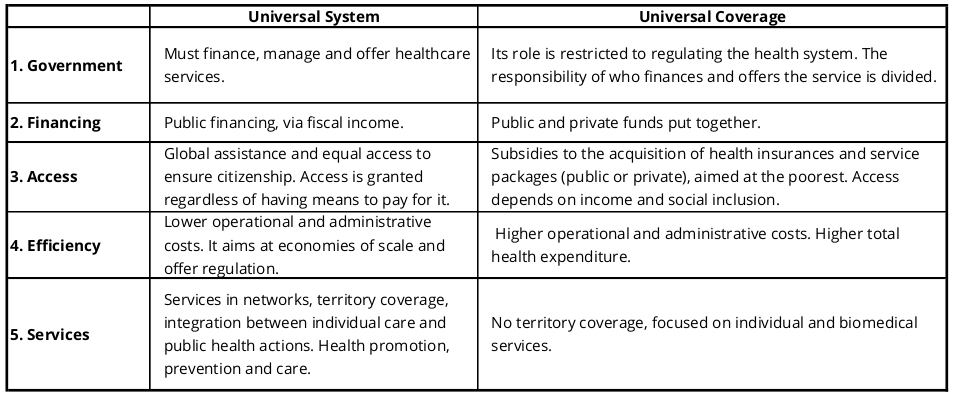
Universal health system and universal health coverage: assumptions and strategies - National School of Public Health, Fiocruz.
Although the Universal Health System seems more equitable and desirable, it converges towards precariousness and even welfarism since it becomes unfeasible to offer that level of investment, reach and quality for all using public resources.
On the other end there is the Universal Health Coverage that, although being based on the organization and efficiency of the private system, tends to mercantilism and may worsen the inequalities, since it focuses on having financial returns from all its initiatives.
Since every polarization is flawed, to move forward with the necessary developments for the health systems and reach the highest level of equity in the distribution of health financial resources, we need well-planned structures that bring together several sources and types of investment.
In the face of complexities caused by modern times and inequalities amassed throughout the years, the international guidance proposes mixed solutions designed among governments and the private initiative.
They rise from the relationships built up beforehand between public and private initiative, since they do not relate the sources of the capital, but attribute different responsibilities to them.
Updating the healthcare service mechanism benefits from a variety of resources, keeping the public and free system addressed exclusively to low and middle-income groups of people, leaving to the market the responsibility to make available subsided health insurance plans and to create health insurances.
It is worth mentioning that developing a public healthcare service exclusive to the low and middle-income population should not be mistaken with low quality, quite the contrary, the initiative aims at gathering the resources to those who cannot have access to the market.
This process requires time, market structuring and a construction structured in stages.
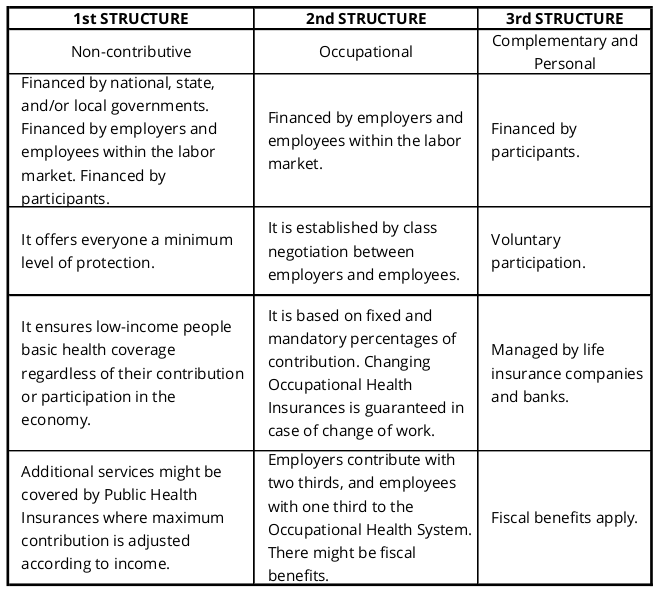
Credit: Claudia Kodja.
Regardless of how we understand citizenship and social rights, the solutions to guarantee financing and access to social services nowadays require a structuring process between public and private sectors. Precariousness and inequality tend to worsen if we cannot see it through.
References
Health at a Glance 2017 - OECD Indicators - access: May/2019 - https://doi.org/10.1787/health_glance-2017-en
KPMG Venture Pulse 2018 - KPMG Enterprise - access: May/2019 - kpmg.com/venturepulse
NCD Slow Motion Disaster - World Healthcare Organization - access: May/2019 - www.who.int/publications/10-year-review/en/
Trends in Healthcare Exits 2018 - Silicon Valley Bank - Authors: Jonathan Norris | Ritish Patnaik
OECD (2017), "Dementia prevalence", in Health at a Glance 2017: OECD Indicators, OECD Publishing - Paris -DOI: https://doi.org/10.1787/health_glance-2017-76-en
World Bank Indicators - https://data.worldbank.org/indicator
Global Health Expenditure Database - https://apps.who.int/nha/database
The Rising Cost of Health Care by Year and Its Causes - See for Yourself If Obamacare Increased Health Care Costs - https://www.thebalance.com/causes-of-rising-healthcare-costs-4064878
Public Spending on Health: A Closer Look at Global Trends - World Healthcare Organization - https://apps.who.int/iris/bitstream/handle/10665/276728/WHO-HIS-HGF-HF-WorkingPaper-18.3-eng.pdf?ua=1
Universal health system and universal health coverage: assumptions and strategies - ISSN 1413-8123On-line version ISSN 1678-4561. Escola Nacional de Saúde Pública, Fiocruz - giovanel@ensp.fiocruz.br.
Spending targets for health: no magic number - World Healthcare Organization - https://apps.who.int/iris/bitstream/handle/10665/250048/WHO-HIS-HGF-HFWorkingPaper-16.1-eng.pdf?sequence=1
About the author
Claudia Kodja
Claudia Kodja graduated from Fundação Getulio Vargas (FGV-SP) and has a PhD in Economic History from Universidade de São Paulo (USP). She wrote the book "Mundo em Crise: a Libertação e o Abandono da Sociedade" (Almedina 2012) and is a certified asset manager by the Brazilian Securities and Exchange Comission (Instrução CVM - nº 306).
contato@kodja.com.br
Send by e-mail:


